Sicker Americans are sticking with Medicare managed care plans
Study finds low rates of switching to traditional Medicare
By Misti Crane
Following decades of criticism for "cherry-picking" the healthiest patients, Medicare managed care plans now appear to be holding onto sicker patients with more complex health needs, new research has found.
The study, which appears today (June 26, 2023) in the Journal of the American Medical Association, found that older Americans with demanding health needs were not more likely to disenroll from Medicare Advantage, the increasingly popular managed care option for Americans age 65 and over.
"This is not what a lot of people would expect, based on what we’ve seen with Medicare managed care plans historically," said senior author Wendy Xu of The Ohio State University’s College of Public Health.
This new study is the first of its kind to look at trends among enrollees with multiple chronic conditions as Medicare Advantage increases in popularity, Xu said, and it doesn’t seem to support the premise that when people get sicker that they become unhappy with care access in the managed care plan and switch to traditional Medicare.
"Twenty or 30 years ago, it used to be that people who develop chronic conditions switch back to traditional Medicare like crazy – but in our study, the switch-back rate was very low," she said.
The research team examined Medicare enrollment data from almost 45,000 enrollees from 2009-2019, when an increasing number of people were opting for Medicare Advantage’s managed care options that more closely mirror the insurance coverage of most working-age Americans.
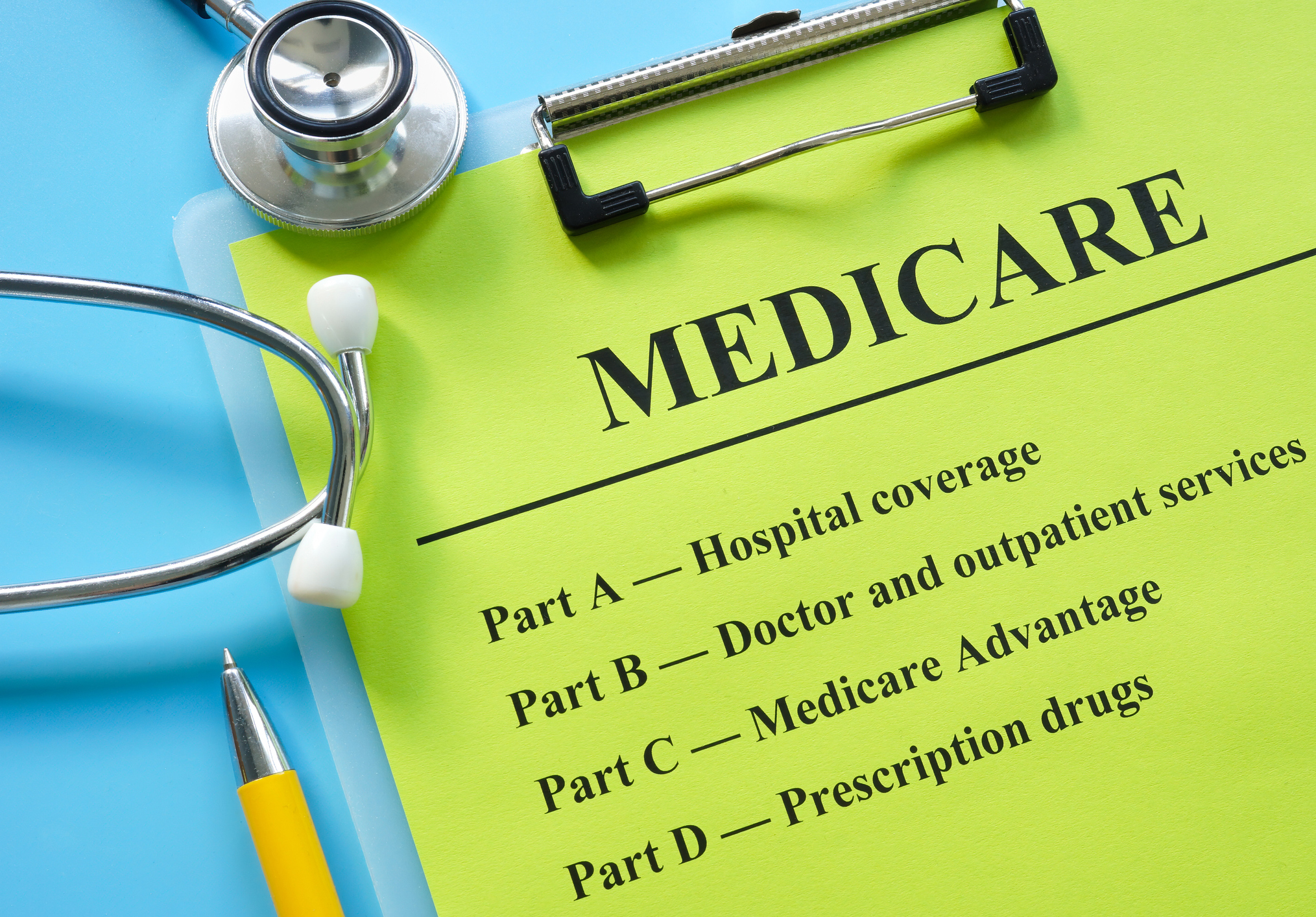
Under these plans, which are operated by private insurance companies, an approved network of health care providers negotiate service rates with the companies. This differs from the traditional fee-for-service Medicare model, in which recipients can see any caregiver who participates in Medicare.
"These plans work with providers to get better rates for their members, so it’s a little more controlled and it also allows for other benefits that you can’t get through traditional Medicare, such as dental care," said Eli Raver, the study’s lead author and a doctoral student at Ohio State’s College of Public Health.
"It tends to have lower premiums and be a bit more coordinated, with an emphasis on the role of primary care, and one of the extra benefits is disease management for multiple conditions, an approach that benefits many aging Americans," Raver said.
About half of Medicare beneficiaries are covered under Medicare Advantage plans and the percentage is rising, Xu said.
"When this model was first created, there was a clear incentive for providers to skimp on health services, and gravitate toward healthier, younger patients. So, the ‘cherry-picking’ criticism was valid," Xu said.
Significant tweaks to Medicare managed care have moved toward a system that better compensates providers for caring for those with complex, chronic conditions.
"These plans have started to enroll a larger proportion of lower-income and minority groups and even people with multiple chronic conditions, and the Medicare program gives them incentives to do that," Xu said.
One notable exception to the study’s findings was among low-income older Americans who are eligible for both Medicare and Medicaid – a highly vulnerable population with demanding health care needs.
"We found that they do have a higher rate of switching from Medicare Advantage to traditional Medicare than non-dual-eligible enrollees," Raver said.
"These plans appear to serve older Americans reasonably well based on our study, but for those with multiple chronic conditions who are also poor, and for those with disabilities, there could be some concerns about whether Medicare Advantage is providing enough access to care."
About The Ohio State University College of Public Health
The Ohio State University College of Public Health is a leader in educating students, creating new knowledge through research, and improving the livelihoods and well-being of people in Ohio and beyond. The College's divisions include biostatistics, environmental health sciences, epidemiology, health behavior and health promotion, and health services management and policy. It is ranked 22nd among all colleges and programs of public health in the nation, and first in Ohio, by U.S. News and World Report. Its specialty programs are also considered among the best in the country. The MHA program is ranked 5th and the health policy and management specialty is ranked 21st.